LAS News
Read article:Three LAS students receive Critical Language Scholarships
Read article:Three LAS students receive Critical Language Scholarships
›
Three LAS students receive Critical Language Scholarships
Department of State program enables 8-10 weeks of studying abroad
Read article:Study identifies atmospheric and economic drivers of global air pollution
Read article:Study identifies atmospheric and economic drivers of global air pollution
›
Study identifies atmospheric and economic drivers of global air pollution
Analysis links emissions to demand and consumption among countries

Read article:
Read article: ›
College of LAS student honored with Goldwater scholarship
Sylvia E, a junior, plans to study early development

Read article:
Read article: ›
College of LAS professor awarded Guggenheim Fellowship
Alison Bell is a pioneer in the study of animal personality

Read article:
Read article: ›
Report: 91 percent of recent LAS alumni secure a first destination soon after graduation
Illini Success initiative surveys graduates during the 2022-23 academic year
Read article:
Read article: ›
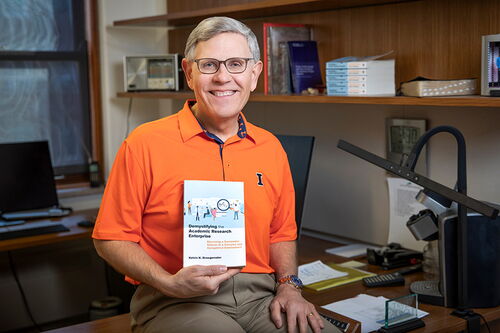
Book: What scholars need to know to thrive in the competitive world of research, creative enterprise
Professor and former science advisor seeks to assist early career professionals

Read article:
Read article: ›
Making room for ideas and innovation
Professors describe how endowed positions expand possibilities for research and scholarship

Read article:
Read article: ›
New method safely extracts gold, platinum, and other metals from waste and low-grade ore
Researchers describe how electrochemistry helps clean up electronic recycling and precious metal mining

Faculty honors
LAS professors bring honor and recognition to the college. See a list of their accomplishments.


Read The Quadrangle and LAS News
The College of Liberal Arts & Sciences mails its magazine, The Quadrangle, twice a year. Its enewsletter, LAS News, mails monthly.







