Beating the odds
Researchers call it the Valley of Death—“the place where drugs go to die,” according to Paul Hergenrother, a University of Illinois chemistry professor.
“Getting through the Valley of Death means you have gone from a drug’s discovery to actually treating the first patient,” he explained. “It’s experimentally challenging, time consuming, and expensive—all of those things.”
Despite the insurmountable odds, after more than 10 years of research, a promising new brain cancer drug from the Hergenrother Lab has made it through this Valley of Death, reaching Phase 1 human clinical trials at the University of Illinois Cancer Center in Chicago and Johns Hopkins Hospital in Baltimore.
What’s more, Hergenrother’s lab was recently awarded an additional $7 million from an “angel investor” (an anonymous donor), on top of an earlier $4 million to fund the research. This award will support the second part of the Phase 1 human trials, as scientists try to gauge tolerable levels of the drug, which is known as PAC-1.
FDA approval is a long and winding road that begins with preclinical testing and moves through three phases of human clinical trials before the new drug application can be filed—a process that can take, on average, eight to 12 years. Hergenrother’s work has reached further than most drug development ideas, but his research is only one of the Department of Chemistry’s many success stories.
Several chemistry professors are working on innovative drug ideas, and the few highlighted here represent three different stages of development. One drug is at an early stage of testing with fruit flies, another is an existing drug found to have clinical use for a different disease, and the third is Hergenrother’s drug, which has moved deeply through the FDA approval process.
Muscular Dystrophy and Molecular Scissors
Just one floor above Hergenrother in Roger Adams Laboratory, fellow chemistry professor Steven Zimmerman has set his sights on a disease with few options—myotonic dystrophy Type 1 (DM1), the most common form of adult onset muscular dystrophy.
“There is no drug on the market for DM1,” Zimmerman said. “A few drugs treat the symptoms but don’t treat the disease itself.” DM1 is a “trinucleotide repeat expansion” disease, meaning that the three repeating nucleotides making up a DNA strand keep repeating themselves, expanding the DNA strand. Expanded DNA creates expanded RNA, which attaches to the muscleblind-like (MBNL) proteins in cells and triggers the symptoms of this form of muscular dystrophy.
Zimmerman’s team is attacking the disease with drug molecules that do three things. First, the molecules prevent expanded DNA from making expanded RNA. Second, they prevent the expanded RNA from binding to the MBNL protein. Finally, “molecular scissors” chop up the expanded RNA, preventing it from doing damage.
“We’re at the stage where the drug is working with fruit flies,” he said. “We’ve seen a significant amount of interest from patients, pharmaceutical companies, start-ups, and venture capital firms, but they all want to see efficacy in mice first.”
Zimmerman and his team discovered this drug possibility purely by chance while they were trying to make DNA bases that bind to other bases more strongly. “It’s like anything in science,” he said. “Sometimes you set off to do one thing, and you stumble onto something else.”
Sand Flies, Kissing Bugs, and Tropical Disease
Teamwork and connections are essential to drug research, as was the case for fellow chemistry professor Eric Oldfield, whose career veered in a new direction after chance encounters with a former M.I.T. classmate, Julio Urbina, researching in Venezuela.
Oldfield had been studying cell membranes, but 15 years ago, after the pair had yet another chance encounter with each other (it was the third time), they finally decided to team up and explore drug ideas for parasitic diseases.
“It got us interested in infectious diseases,” Oldfield said.
They began by working on treatment ideas for leishmaniasis, which is spread in tropical regions by bites from infected sand flies. Leishmaniasis can leave horrific lesions on a person’s body, and a more deadly version of the disease attacks internal organs, such as the spleen or liver.
They discovered that an existing heart drug, amiodarone, kills the parasitic protozoa that causes leishmaniasis. In South America, amiodarone is now being used clinically for patients with the skin disease. In addition, it is the only drug available for patients suffering from both leishmaniasis and Chagas disease, an ailment that affects the heart. Chagas disease is transmitted by “kissing bugs” that live in the crevices of walls, coming out at night to bite sleeping people on the face. It sounds like something out of a horror movie, but amiodarone has eased some of the fear.
Drug discovery is very much a team effort, which is why Oldfield collaborates with so many researchers—most recently with the Salk Institute—in an effort to develop a drug targeting lung cancer cells. In addition, his lab is exploring a new drug against tuberculosis. It’s a massive team effort as seen in a recent scientific paper with 26 co-authors.
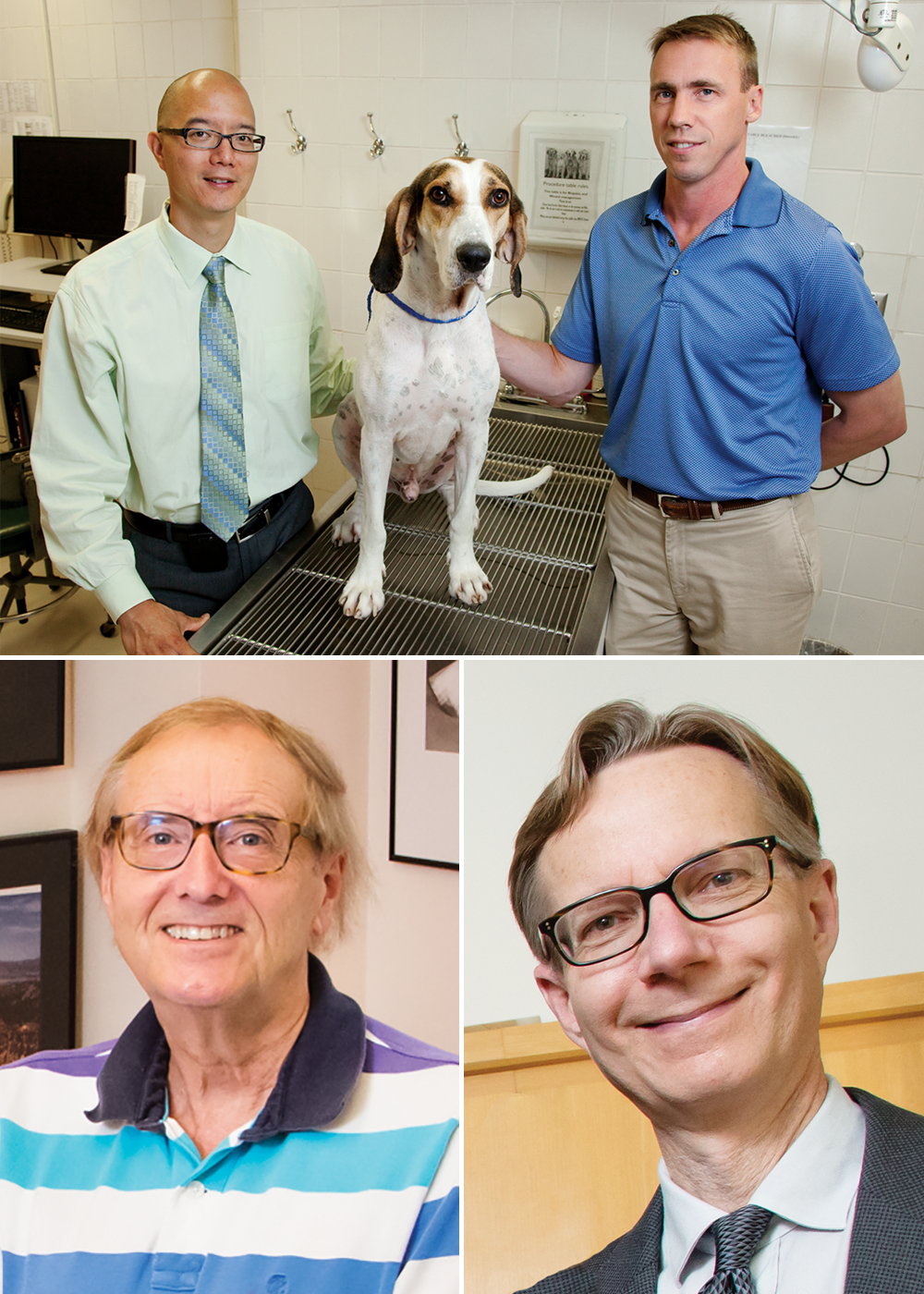
The Canine and Cat Connection
For Hergenrother, teamwork was also the key to their success. It took a one-of-a-kind collaboration with the U of I College of Veterinary Medicine to bring the lab’s PAC-1 drug so far along in the testing process. Ten years ago, after Hergenrother released the first results on PAC-1, Illinois veterinary oncologist Timothy Fan approached him and suggested they test the drug on dogs that came into the U of I veterinary clinic with various forms of cancer. The dogs contracted cancer naturally and have no other options. Without the PAC-1 treatment, they would have been euthanized.
“These dogs are real cancer patients,” Hergenrother said. “They have been exposed to all the same toxins that you and I are, and in many cases they come down with cancers that are very similar to the human disease. We believe that compounds that show efficacy in these veterinary cancer patients will have a much better chance of working in human clinical trials.”
The drug offers new hope for human cancer patients who have no other options left. PAC-1 has the ability to penetrate the brain to get at the tumor, which not many drugs can do. TMZ is the current drug used for a deadly form of brain cancer known as glioblastoma meningioma, but it gives patients only months of additional survival. (The median survival rate for this disease is 14 months.) The hope is that PAC-1, alone or in combination with TMZ, will boost that rate significantly.
Building on the research using PAC-1 on canine cancer patients, Hergenrother, Fan, and two other U of I professors—Jun Song and Pablo Perez-Pinera in bioengineering—have teamed up to form the Anticancer Discovery from Pets to People group in the Institute for Genomic Biology. Hoping to duplicate the success in dogs, this group has expanded the work to include cats.
Hergenrother and his colleagues developed a promising new drug, DNQ, that treats an oral cancer in cats similar to head and neck cancer in humans. It has a ways to go before getting through the Valley of Death.
Even when a drug candidate makes it through the valley, there remains a long road ahead. As Hergenrother said, “We’re through the Valley of Death with PAC-1, but that doesn’t mean we’re out of the woods.”
This story appeared in the Fall 2016 LAS News magazine (PDF).